Surgery for Sinusitis
WHAT IS FUNCTIONAL ENDOSCOPIC SINUS SURGERY (FESS)?
One way functional endoscopic sinus surgery differs from conventional sinus surgery is that an endoscope is used in the nose to view the nasal cavity and sinuses. This generally eliminates the need for an external incision. The endoscope allows for better visualization of diseased or problem areas. This endoscopic view, along with detailed radiological studies, may reveal a problem that was not evident before.
Functional endoscopic sinus surgery focuses on treating the underlying cause of the problem. The sinuses can be viewed directly and obstructive tissue removed if necessary. There is often better preservation of normal tissue, and the surgery can frequently be performed on an outpatient basis.
WHEN IS ENDOSCOPIC SINUS SURGERY INDICATED?
Endoscopic sinus surgery is generally intended for people with chronic sinus problems that do not respond to medical therapy. The majority of people with sinusitis do not require surgery. Their sinus symptoms can usually be successfully treated medically with an antibiotic, and other medicines used to reduce inflammation. The type of medical therapy used is based on the best clinical assessment of the possible cause(s). Maximal medical therapy is typically initiated to see how you respond to treatment before deciding on a surgical procedure. If it is felt that you would benefit from endoscopic sinus surgery, I will recommend the procedure.
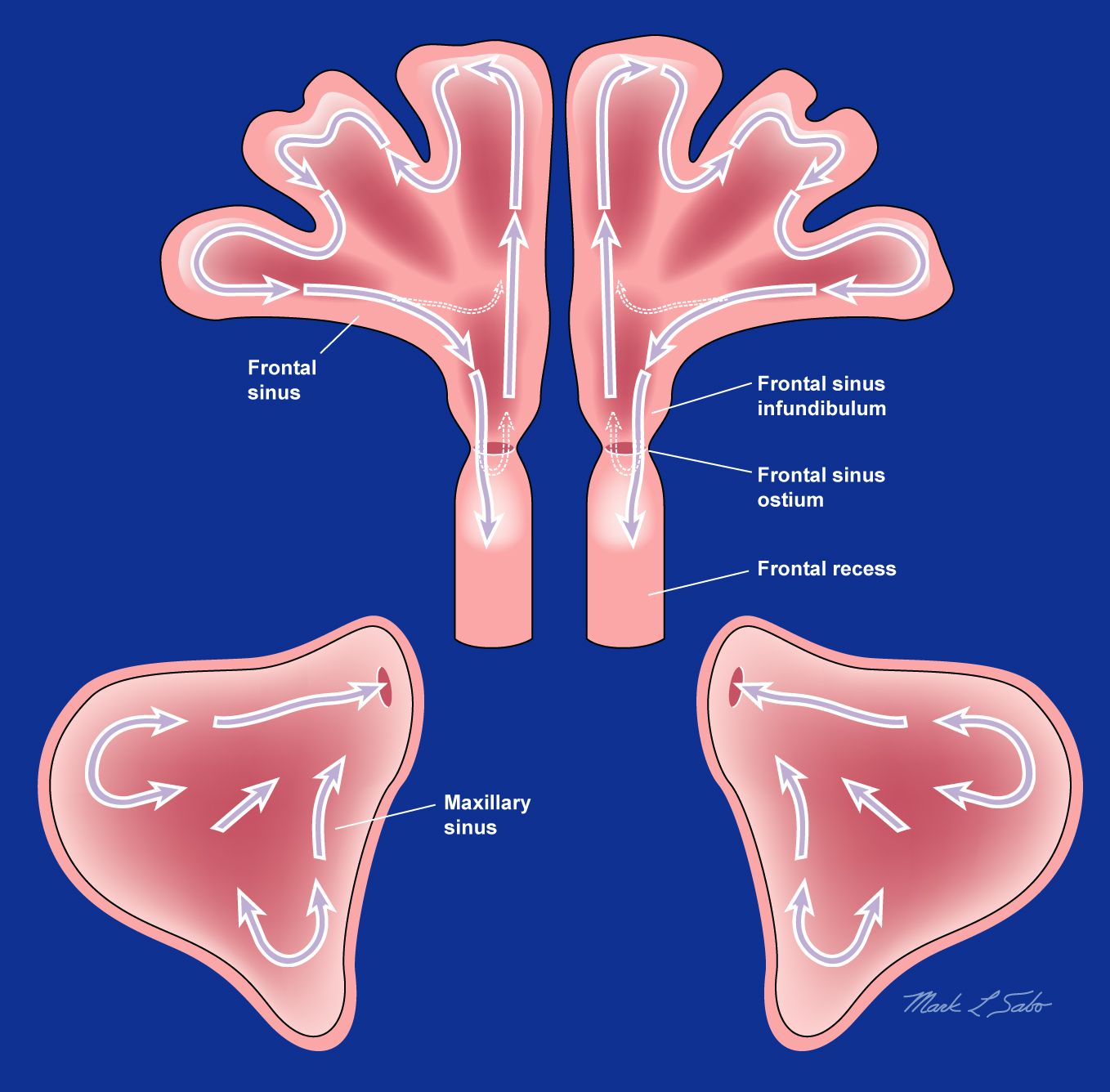
Surgery is indicated if an infected or inflamed area does not clear with antibiotic therapy or other medications, or because the symptoms keep returning when antibiotics are stopped. The primary goal of the sinus surgery is to restore drainage of the sinuses and to facilitate the return of normal functioning of the lining of the sinuses (mucociliary clearance). Additionally, open sinus passages can help better define possible causes of recalcitrant or chronic sinus disease. The tissue is sent to the pathologists and secretions are often sent for culture to identify if bacteria or fungus are present. Post-operatively surgical openings improve access of the sinuses to irrigation which can help keep the sinuses clean and improve their functioning.
WILL ENDOSCOPIC SINUS SURGERY CURE MY SINUS PROBLEMS?
Chronic rhinosinusitis is rarely cured by this intervention but it is made to be significantly improved. It should be realized that some medical therapy is typically continued after surgery, especially if allergy or polyps play a role. This is necessary to minimize or prevent recurrence of disease. When surgery is performed for chronic rhinosinusitis, wound healing and sinus improvements can be gradual and take more than one year before they improve to their best condition.
Overall, the majority of patients have had significant improvement with the combination of surgery and continued medical management. We will certainly work with you to attain this goal.
What is the Frontal Sinus Drill-Out (DRAF 3 / Modified Lothrop Procedure) ?
The frontal sinus drill-out is a completely endoscopic intranasal technique that creates a common communication between the frontal cavities and the nose in order to fix improper drainage of the frontal sinuses. It is an advanced surgical alternative which establishes functionality rather than open obliteration procedures in which the cavity is eradicated. This technique provides excellent visualization of the frontal sinus in the postoperative setting for adequate monitoring. In expert hands, this procedure can be safe and highly effective in the management of serious frontal sinus problems.
For a demonstration of the system press this link
The Stealth Neuronavigation System
The use of a navigation system is intended as an aid for locating anatomical structures and planning surgical trajectories in endoscopic procedures. Using image-guided surgery can enable more precise and safer endoscopic sinus surgery. This technology has become an industry standard for many endoscopic sinus surgeries. The American Academy of Otolaryngology – Head and Neck Surgery (AAO-HNS) endorses the use of image-guided surgery for procedures including:
- Revision sinus surgery
- Distorted sinus anatomy of development, postoperative, or traumatic origin
- Extensive sino-nasal polyposis
- Pathology involving the frontal, posterior ethmoid and sphenoid sinuses
- Disease abutting the skull base, orbit, optic nerve, or carotid artery
- CSF rhinorrhea or conditions where there is a skull base defect
- Benign and malignant sino-nasal neoplasms
For a demonstration of the system press this link
What is the steroid-eluting biological implant?
After opening the sinus during surgery, the physician places a steroid-eluting biological implant in the sinus. The spring-like design of the implant allows it to conform to the unique shape of the cavity. It stays securely in place and props it open. Over the next 30 days, the implant is designed to deliver a sustained release of mometasone furoate over the surfaces. The anti-inflammatory properties of the PROPEL® Sinus Stent is proven to improve the effectiveness of surgery by keeping the sinuses open. The implant dissolves itself in approximately 30 to 45 days, however in many occasions depending on the healing process I may remove it earlier. It is lightweight, and usually cannot be felt once in place.
This advanced technology has clinically proven to improve success following surgery by:
- Reducing scarring of the healing sinus by 70%
- Reducing the need for additional post-surgery interventions and oral steroid medications by 35%.
- Reducing polyp formation by 46%.
Han JK, Marple BF, Smith TL, et al. Int Forum Allergy Rhinol. 2012; 2:271-279.
For a demonstration of the device press this link
What is Balloon Sinuplasty?
Balloon Sinuplasty (BSP) uses a small, flexible, balloon catheter to open up blocked sinus passageways to relieve pressure and pain in patients suffering from chronic sinusitis symptoms.
It is a minimally invasive office procedure, performed under local anesthesia, which can re-established sinus drainage. It is a viable option for patients with limited sinus disease or for those patients with multiple health comorbidities in which general anesthesia is not an option. For the right patient, this procedure can be beneficial.