Endoscopic Applications in Orbital Surgery
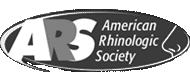
Dacryocystorhinostomy
LACRIMAL SYSTEM
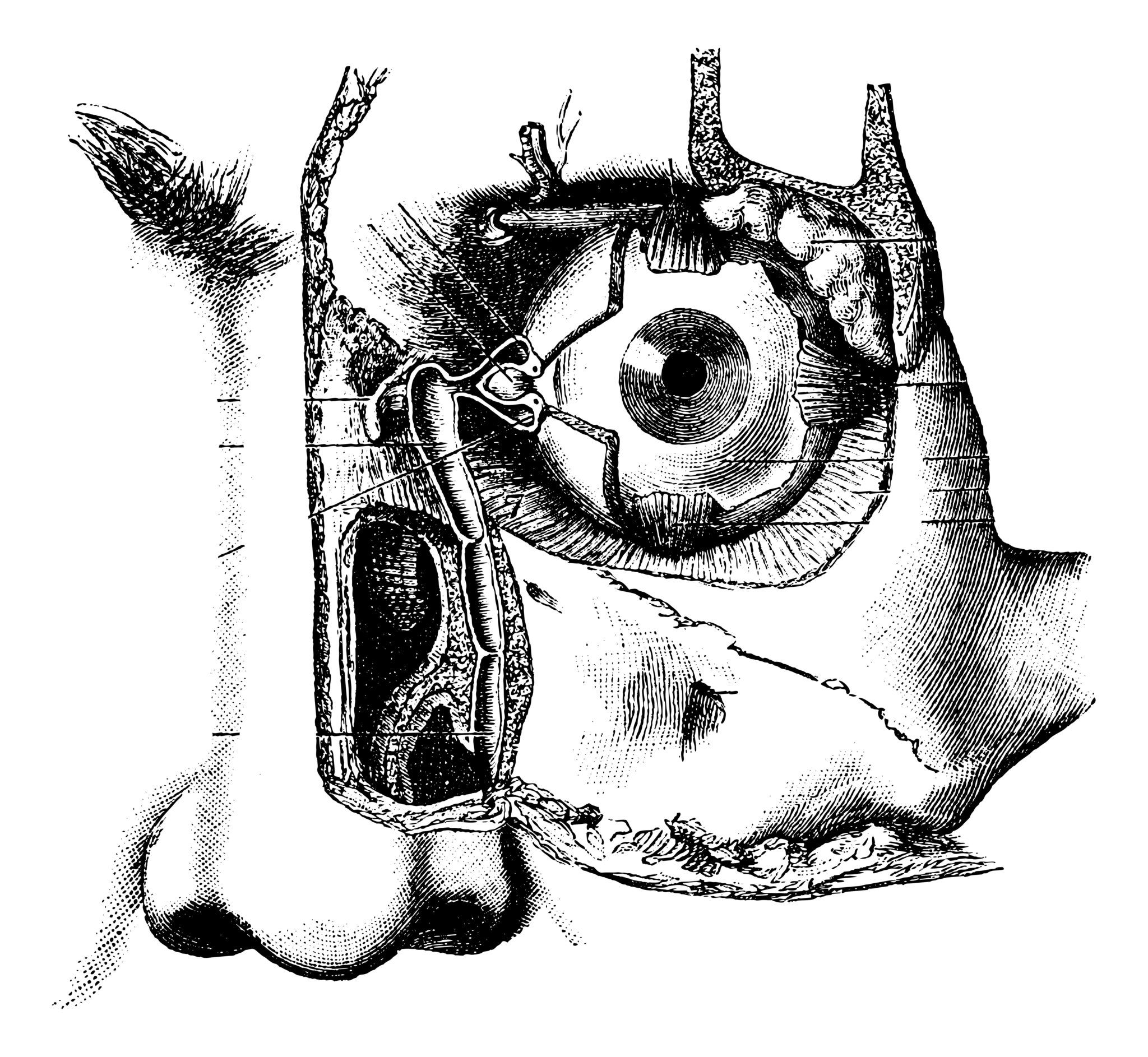
Tears are created by the lacrimal gland and after lubricating the eye they flow through a lacrimal system into the nose. The lacrimal system consists of the canaliculus, the lacrimal sac and the nasolacrimal duct. Acquired nasolacrimal duct obstruction can occur as a result of maxillofacial trauma, sinus disease or systemic inflammatory disease. The common symptoms of nasolacrimal obstruction are epiphora (abnormal tearing) and dacryocistitis (infection lacrimal sac) and the definitive treatment requires a surgical procedure which connects the lacrimal sac directly into the nasal cavity bypassing the nasolacrimal duct. This surgical procedure is known as dacryocystorhinostomy (DCR) and has been traditionally performed through external approaches with excellent results.
A modern technique is the transnasal endoscopic approach which has the advantage of avoiding skin incisions and scars. In addition, the endoscopic approach preserves the pumping mechanism of the orbicularis oculi muscle and produces less disruption of the medial canthal anatomy.
Orbital Wall Decompression
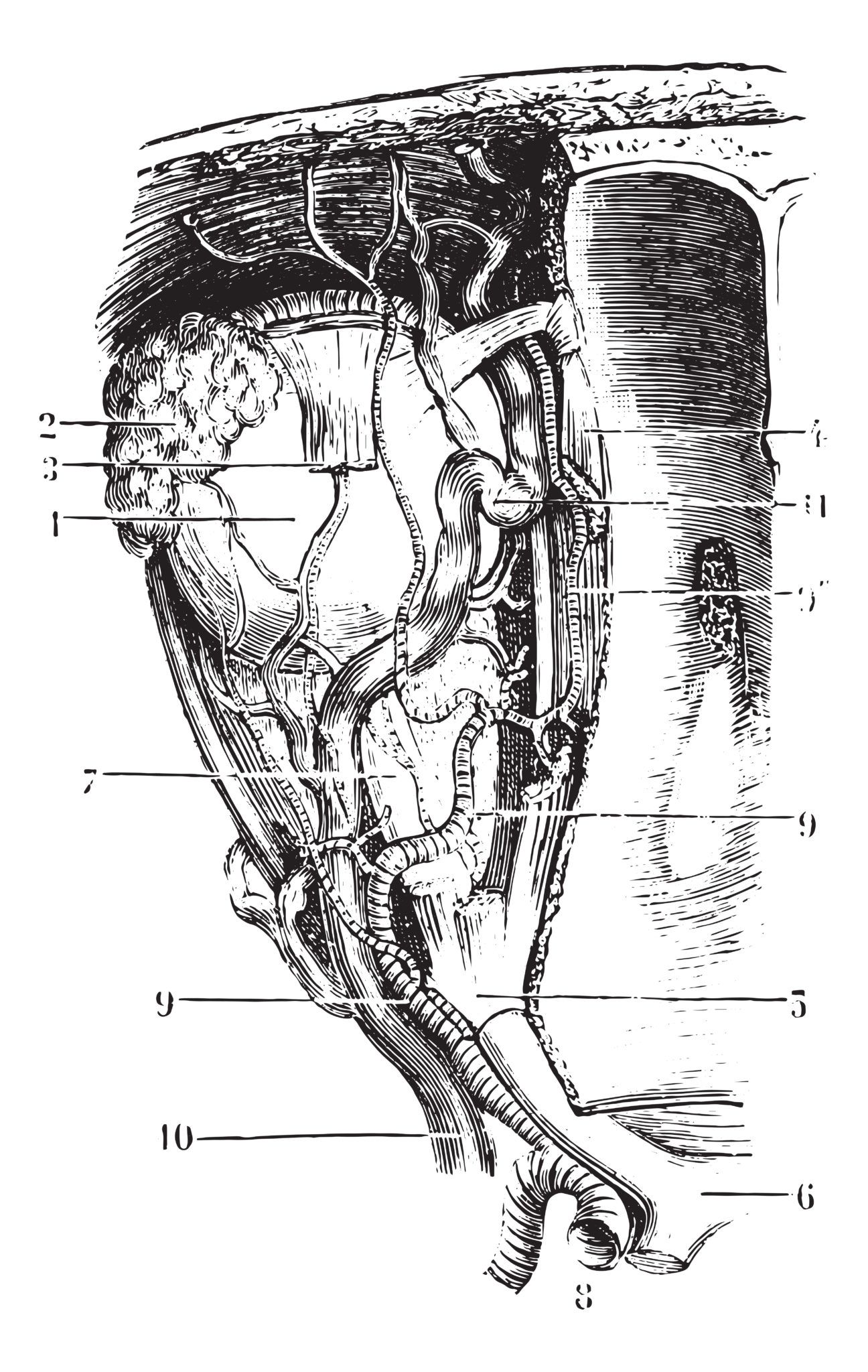
ORBIT
Thyroid eye disease (also known as Graves’ ophthalmopathy or thyroid related ophthalmopathy) is the most common cause of proptosis in adults. It is considered an autoimmune process in which the thyroid-stimulating hormone (TSH) receptor is the likely target in both the thyroid gland and orbit. Fibroblasts are attracted to these areas inducing a severe inflammatory response.
Symptoms of thyroid eye disease include blurred vision, foreign body sensation, photophobia, tearing, double vision and pain. Clinically patients present with eyelid retraction, periorbital swelling, restrictive myopathy and exophthalmos. In some cases the severity of the disease can cause optic neuropathy and visual loss. When indicated surgical rehabilitation is usually staged with orbital decompression first, followed by strabismus surgery, and finally, eyelid surgery.
Nonsurgical Management of Thyroid Eye Disease
Thyroid eye disease is usually self-limited and the majority of patients require only supportive care, including aggressive ocular lubrication, cool compresses, and eye protection measures. Managing and controlling the thyroid gland dysfunction is the first step to reverse the orbitopathy. Systemic steroids and Selenium supplementation are the most commonly use pharmacotherapeutic agents. A more controversial option is the use of radiation which has shown inconsistent results.
Surgical Management of Thyroid Eye Disease
Surgical decompression of the orbit is a validated treatment of thyroid eye disease. Indications include compressive optic neuropathy, exposure keratopathy, and disfiguring proptosis. Surgical approaches for decompressing the orbit include trans cranial, bicoronal flap, transconjunctival transantral, and the minimally invasive endonasal technique. The degree of recession of the exophthalmos achieved by orbital decompression is directly related to the number of walls surgically decompressed.
Optic Nerve Decompression
OPTIC NERVE CANAL
The optic nerve is divided into four segments: intraocular, intraorbital, intracanalicular, and intracranial segments. The typical target of endoscopic optic nerve decompression is the intracanalicular segment. Endoscopic optic nerve decompression requires significant experience with advanced rhinologic techniques, innovative technology available and a multidisciplinary team which includes a Rhinologist and an Ophthalmologist.
The most common indication for this procedure is traumatic optic neuropathy. The procedure has shown benefits on patients with compressive optic neuropathy related to tumors, osseous lesions or thyroid orbitopathy. Finally, the benefits of this surgery on patients with idiopathic intracranial hypertension was recently published in the International Forum of Allergy and Rhinology by Tarrats et al.